Depression and chronic pain are two complex conditions that often coexist, with research indicating a strong connection between the two. This relationship has garnered significant attention in the medical field due to its profound impact on individuals' well-being and quality of life.
The prevalence of depression in people experiencing chronic pain is remarkably high, suggesting a potential link between the two conditions. Furthermore, various biological mechanisms, such as alterations in neurotransmitters and the immune system, have been identified as potential contributors to this connection.
In addition, psychological factors, including negative thought patterns and reduced coping abilities, play a significant role in the relationship between depression and chronic pain. Understanding the intricate interplay between these conditions is crucial in developing effective treatment approaches that address both mental health and pain management.
The Prevalence of Depression in Chronic Pain
The prevalence of depression in individuals experiencing chronic pain is a significant concern, as studies have consistently demonstrated a strong association between the two conditions. Research has shown that individuals with chronic pain are more likely to experience symptoms of depression compared to those without chronic pain.
In fact, a systematic review and meta-analysis conducted by Bair et al. (2003) found that the prevalence of depression in chronic pain patients ranged from 30% to 54%. Furthermore, a longitudinal study by Ohayon and Schatzberg (2003) revealed that individuals with chronic pain were more than twice as likely to develop depression compared to those without chronic pain.
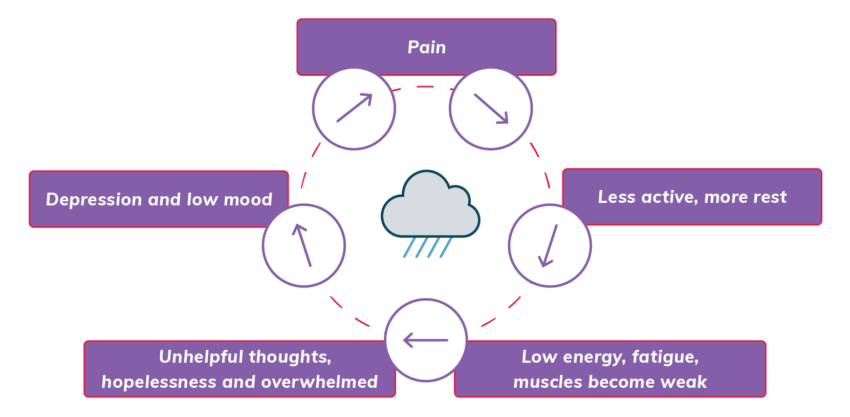
The relationship between depression and chronic pain is complex and bidirectional. Chronic pain can lead to feelings of hopelessness, despair, and loss of enjoyment in activities, which are characteristic symptoms of depression. On the other hand, individuals with depression may be more sensitive to pain and have a lower pain tolerance.
This bidirectional relationship reinforces the need for a comprehensive approach in managing both conditions. It is important for healthcare professionals to screen and assess individuals with chronic pain for symptoms of depression regularly. Early detection and intervention can help improve the overall well-being and quality of life for these individuals.
Additionally, a multidisciplinary approach that includes addressing both the physical and psychological aspects of chronic pain is crucial in effectively managing and treating these conditions.
Biological Mechanisms Linking Depression and Chronic Pain
The interplay between depression and chronic pain involves complex biological mechanisms. While the exact mechanisms are not fully understood, several theories have been proposed to explain the link between these two conditions.
One theory suggests that alterations in neurotransmitter systems, such as serotonin and norepinephrine, play a crucial role. Both depression and chronic pain have been associated with imbalances in these neurotransmitters, which can affect mood and pain perception.
Additionally, chronic pain can lead to changes in the structure and function of the brain, including areas involved in emotional regulation and pain processing. These changes may contribute to the development or maintenance of depressive symptoms.
Another proposed mechanism involves the activation of the immune system. Chronic pain can trigger an immune response, leading to the release of pro-inflammatory cytokines. These cytokines can then affect the brain and contribute to the development of depressive symptoms.
Furthermore, genetics may also play a role in the relationship between depression and chronic pain. Studies have shown that certain genetic variations may increase the risk of developing both conditions.
The Impact of Depression on Pain Perception
Frequently, depression significantly influences the perception of pain. This impact can be attributed to various factors that interact and contribute to the overall experience of pain.
- Altered brain chemistry: Depression leads to changes in neurotransmitters, such as serotonin and norepinephrine, which can heighten pain sensitivity and decrease pain tolerance.
- Heightened stress response: Depression is often accompanied by an overactive stress response, which can amplify pain signals and make them more intense.
- Negative cognitive biases: Depressed individuals tend to have negative thoughts and beliefs about their pain, which can exacerbate their experience of pain and make it feel more intense.
Research has consistently shown that individuals with depression tend to report higher levels of pain and discomfort compared to those without depression.
Furthermore, the presence of depression can also worsen the prognosis and treatment outcomes for individuals with chronic pain conditions. It is crucial to address both depression and pain simultaneously in order to effectively manage and alleviate the suffering experienced by individuals with comorbid depression and chronic pain.
Psychological Factors Influencing the Relationship Between Depression and Chronic Pain
Psychological factors significantly influence the relationship between depression and chronic pain. Research has shown that individuals with depression are more likely to experience chronic pain, and vice versa. Several psychological factors contribute to this complex relationship.
Firstly, negative thinking patterns play a crucial role. Individuals with depression often have negative thoughts and beliefs about themselves, others, and the world. These negative thoughts can exacerbate pain perception and lead to increased pain intensity and duration. Additionally, catastrophizing, which involves magnifying the significance of pain and anticipating negative outcomes, is commonly observed in individuals with both depression and chronic pain.
Secondly, emotional factors such as stress, anxiety, and fear can intensify the experience of pain. These emotions can heighten pain sensitivity and make it more difficult to cope with chronic pain. Moreover, individuals with depression may have difficulty regulating their emotions, which can further amplify pain perception.
Lastly, social factors, including social support and social isolation, can influence the relationship between depression and chronic pain. Lack of social support can increase feelings of loneliness and exacerbate depressive symptoms, which in turn can impact pain perception.
Treatment Approaches for Managing Depression and Chronic Pain
Several effective treatment approaches exist for managing both depression and chronic pain. These approaches aim to address the physical and psychological aspects of these conditions, providing relief and improving overall well-being.
Here are three treatment approaches that have shown promise:
- Medication: Antidepressants are commonly prescribed to manage both depression and chronic pain. These medications can help regulate mood and alleviate pain symptoms. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are often prescribed for their dual benefits in treating depression and chronic pain.
- Therapy: Cognitive-behavioral therapy (CBT) has been widely used in the treatment of both depression and chronic pain. CBT helps individuals identify and challenge negative thoughts and behaviors, promoting healthier coping strategies. Additionally, acceptance and commitment therapy (ACT) can help individuals accept their pain and focus on meaningful activities and values.
- Physical interventions: Physical therapies such as exercise, physiotherapy, and acupuncture can be beneficial for managing both depression and chronic pain. Exercise releases endorphins, which can improve mood and reduce pain. Physiotherapy can help improve physical function and reduce pain, while acupuncture has been shown to provide pain relief and improve psychological well-being.
These treatment approaches can be used individually or in combination, depending on the severity and specific needs of the individual. It is important to consult with healthcare professionals to determine the most appropriate treatment plan.
Frequently Asked Questions
Can Chronic Pain Cause Depression?
Chronic pain can indeed cause depression. The continuous physical discomfort experienced by individuals can lead to feelings of hopelessness, helplessness, and low mood. The relationship between chronic pain and depression is complex and often requires a multidisciplinary approach for effective management.
What Are Some Common Psychological Factors That Can Worsen the Relationship Between Depression and Chronic Pain?
Common psychological factors that can worsen the relationship between depression and chronic pain include anxiety, stress, negative thinking patterns, social isolation, and a lack of social support. These factors can exacerbate both conditions and hinder recovery.
Is There a Specific Age Group That Is More Susceptible to Experiencing Both Depression and Chronic Pain?
Certain age groups may be more susceptible to experiencing both depression and chronic pain. Identifying these age groups can aid in developing targeted interventions and treatment plans to improve the overall well-being and quality of life for individuals affected by these conditions.
Are There Any Lifestyle Changes That Can Help Manage Both Depression and Chronic Pain?
There are lifestyle changes that can help manage both depression and chronic pain. These may include regular exercise, healthy diet, stress management techniques, adequate sleep, social support, and engaging in activities that bring joy and fulfillment.
Can Depression Be a Symptom of Chronic Pain Rather Than a Separate Condition?
Depression can be a symptom of chronic pain rather than a separate condition. Research suggests that the experience of chronic pain can lead to the development of depression due to the psychological, physiological, and social factors involved.